Medical Office
Staff
- Psychiatrist:12
- Full-time Internal Medicine:1
- Part-time Internal Medicine: 2
- Surgeon:1
Our Hospital’s Psychiatric Rehabilitation Idea
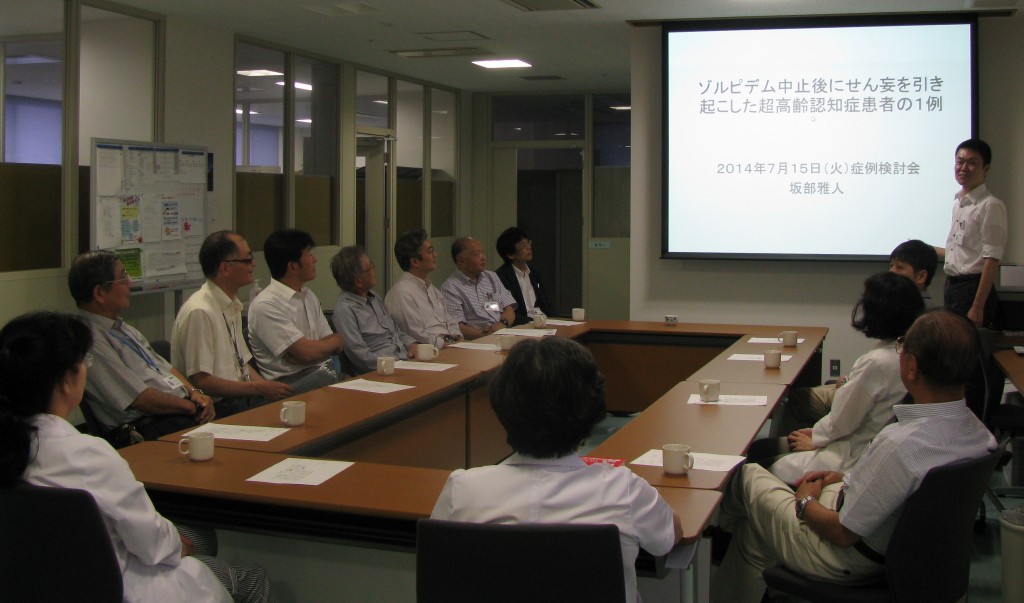
As it is visible in the graph above, for patients who have a mental illness, the stimulation vs. response curve is a lot lower than that of a “Healthy Control”. From this we believe that for a mentally ill individual, compared to an unimpaired individual, it is more difficult to increase the performance level per increase in level of arousal. In other words we hypothesize that, for a patient, by increasing the level of arousal, their performance reaches its peak at an earlier stage (Point C), and thus reaches failure at an earlier stage (Point C). Our ideal psychiatric rehabilitation effect is to shift this stimulation vs. response curve to that of an unimpaired individual curve (B’-B) as much as possible.
Implementation of SST into Various Psychiatric Rehabilitation Activities
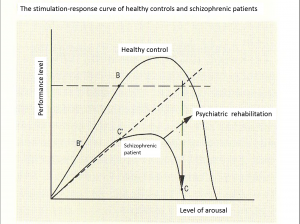
Figure. We have at least four different SST classes: 1) Nishikawa Open Model for in- and outpatients, 2) Closed Model lead by the nursing department for inpatients, 3) Semi-open Model for daycare members, and 4) Closed Model for members participating to the working continuation support program.
We are one of the first psychiatric hospitals (Year. 1991) in Japan to implement SST (social skills training), which was introduced by Liberman, into our hospital’s medical practice. Since we believe that SST is one of the best methods to “correct” the stimulation vs. response curve, not only do we use SST for hospitalized patients, we also include this method in our daycare services as well as for clients participating in the employment support program; implementing SST for a wide variety of psychiatric rehabilitation. By combining these society return support programs with SST, we strengthen our patients’ tolerance to stress, and thus increasing the number of patients who can return to their normal life routines.
Judo Treatment
Judo is a combination of the martial art“Ju-jitsu,” which was created in the 12th century by bushi warriors, and the philosophies of “Zen”. Today, it is an Olympic Sport and is enjoyed by people all around the world. We believe that Judo is an effective psychiatric rehabilitation; not only does it strengthen the body, but Judo also improves self-control, concentration, and teamwork. Our hospital’s judo class, which only includes the essences of judo, is a 1 hour class where both patients and employees can have fun in a club like fashion. Our motto is “it is not about winning, but to enjoy judo in your natural form”, and our class is not a place for intense training. There are many cases where this judo treatment had positive results in the treatment of patients with depression and schizophrenia. We hypothesise that the response mechanism for the judo treatment to be, 1) judo activates not the head (frontal lobe) but the extrapyramidal system (dopamine system), 2) increases willpower (dopamine system) through “battle”, 3) activates reward system (dopamine system) by praising beautiful techniques.
Clinical Research
Major research interests at Nishikawa Hospital
- Antipsychotic-induced extrapyramidal and other related side effects
- Water-intoxciation in schizophrenic patients
- Prophylactic study of schizophrenia
1: Nishikawa T, Araki Y, Hayashi T. Intractable hiccups (singultus) abolished by risperidone, but not by haloperidol. Ann Gen Psychiatry. 2015 14:13. doi: 10.1186/s12991-015-0051-5. eCollection 2015.
2: Hayashi T, Legati A, Nishikawa T, Coppola G. First Japanese family with primary familial brain calcification due to a mutation in the PDGFB gene: an exome analysis study. Psychiatry Clin Neurosci. 2015 69(2):77-83.
3: Nishikawa T, Hayashi T, Koga I, Uchida Y. Neuroleptic withdrawal with remitted schizophrenics: a naturalistic follow-up study. Psychiatry. 2007 70(1):68-79.
4: Matsumoto T, Mizuno S, Tsukada J, Inami Y, Horiguchi J. Effect of risperidone of polysomnography in healthy subjects. Sleep Biol Rhythm. 2007 5:146-148.
5: Hayashi T, Nishikawa T, Koga I, Uchida Y, Horiguchi J, Yamawaki S. Involvement of the alpha2-adrenergic system in polydipsia in schizophrenic patients: a pilot study. Psychopharmacology (Berl). 1997 130(4):382-6.
6: Tawara Y, Nishikawa T, Koga I, Uchida Y, Yamawaki S. Transient and intermittent oral dyskinesia appearing in a young woman ten days after neuroleptic treatment. Clin Neuropharmacol. 1997 20(2):175-8.
7: Hayashi T, Nishikawa T, Koga I, Uchida Y, Yamawaki S. Prevalence of and risk factors for respiratory dyskinesia. Clin Neuropharmacol. 1996 19(5):390-8.
8: Hayashi T, Nishikawa T, Koga I, Uchida Y, Yamawaki S. Life-threatening dysphagia following prolonged neuroleptic therapy. Clin Neuropharmacol. 1997 20(1):77-81.
9: Nishikawa T, Tsuda A, Tanaka M, Nishikawa M, Koga I, Uchida Y. Involvement of the endogenous opioid system in the drinking behavior of schizophrenic patients displaying self-induced water intoxication: a double-blind controlled study with naloxone. Clin Neuropharmacol. 1996 19(3):252-8.
10: Nishikawa T, Tsuda A, Tanaka M, Nishikawa M, Koga I, Uchida Y. Decreased polydipsia in schizophrenic patients treated with naloxone. Am J Psychiatry. 1994 151(6):947.
11: Nishikawa T, Tsuda A, Tanaka M, Nishikawa M, Koga I, Uchida Y. Naloxone attenuates drinking behavior in psychiatric patients displaying self-induced water intoxication. Prog Neuropsychopharmacol Biol Psychiatry. 1994 18(1):149-53.
12: Nishikawa T, Tsuda A, Tanaka M, Nishikawa M, Koga I, Uchida Y. Naloxone attenuates drinking behavior in a schizophrenic patient displaying self-induced water intoxication. Clin Neuropharmacol. 1992 15(4):310-4.
13: Nishikawa T, Kaneda W, Uegaki A, Koga I, Uchida Y, Tanaka M. Respiratory dyskinesia: a variety of clinical forms differentially diagnosed by using a spirograph. Clin Neuropharmacol. 1992 15(4):315-21.
14: Nishikawa T, Yamada S, Tsuda A, Tanaka M, Koga I, Uchida Y. Chronic treatment with talipexole dihydrochloride on abnormal involuntary movement in humans. Clin Neuropharmacol. 1990 13(3):259-63.
Basic Neuroscience Research
Major Research Interests at Nishikawa Hospital
- Molecular mechanisms of the sigma receptor
- Cellular stress and psychiatric disorders
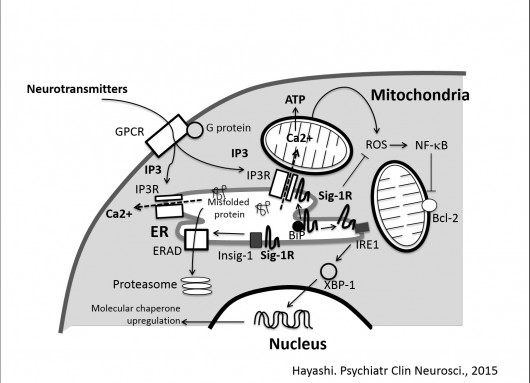
Figure. Roles of the sigma-1 receptors in cellular stress
Sigma-1 receptors are localized at ER membranes associated with mitochondria (MAM). The sigma-1 receptor in the complex with ER chaperone BiP is in active state as a molecular chaperone. Upon binding of sigma-1 receptor agonists or decrease of ER Ca2+, the sigma-1 receptor dissociate from BiP and stabilize IP3 receptors or IRE1 as an active molecular chaperone. The stabilization of IP3 receptors may contribute to Ca2+ transfer to mitochondria and ATP synthesis, whereas the stabilization of IRE1 may promote long-lasting activation of IRE1-XBP-1 pathway and ameliorate ER stress. The sigma-1 receptor is involved in ERAD, especially that regulating degradation of Insig-1 binding lipid enzymes. Though the molecular mechanism is unknown, sigma-1 receptors also ameliorate oxidative stress by negatively regulating accumulation of ROS. The action results in the intrinsic suppression of NF-kB activities and upregulation of anti-apoptotic protein Bcl-2.
1: Hayashi T. Sigma-1 receptor: the novel intracellular target of neuropsychotherapeutic drugs. J Pharmacol Sci. 2015 127(1):2-5.
2: Hayashi T. Conversion of psychological stress into cellular stress response: roles of the sigma-1 receptor in the process. Psychiatry Clin Neurosci. 2015 69(4):179-91.
3: Kourrich S, Hayashi T, Chuang JY, Tsai SY, Su TP, Bonci A. Dynamic interaction between sigma-1 receptor and Kv1.2 shapes neuronal and behavioral responses to cocaine. Cell. 2013 17;152(1-2):236-47.
4: Hayashi T, Hayashi E, Fujimoto M, Sprong H, Su TP. The lifetime of UDP-galactose:ceramide galactosyltransferase is controlled by a distinct endoplasmic reticulum-associated degradation (ERAD) regulated by sigma-1 receptor chaperones. J Biol Chem. 2012 287(51):43156-69.
5: Su TP, Hayashi T, Maurice T, Buch S, Ruoho AE. The sigma-1 receptor chaperone as an inter-organelle signaling modulator. Trends Pharmacol Sci. 2010 31(12):557-66.
6: Tsai SY, Hayashi T, Harvey BK, Wang Y, Wu WW, Shen RF, Zhang Y, Becker KG, Hoffer BJ, Su TP. Sigma-1 receptors regulate hippocampal dendritic spine formation via a free radical-sensitive mechanism involving Rac1xGTP pathway. Proc Natl Acad Sci U S A. 2009 106(52):22468-73.
7: Su TP, Hayashi T, Vaupel DB. When the endogenous hallucinogenic trace amine N,N-dimethyltryptamine meets the sigma-1 receptor. Sci Signal. 2009 2(61):pe12. doi: 10.1126/scisignal.261pe12.
8: Hayashi T, Rizzuto R, Hajnoczky G, Su TP. MAM: more than just a housekeeper. Trends Cell Biol. 2009 19(2):81-8.
9: Hayashi T, Su TP. Sigma-1 receptor chaperones at the ER-mitochondrion interface regulate Ca(2+) signaling and cell survival. Cell. 2007 131(3):596-610.
10: Uchida N, Ujike H, Tanaka Y, Sakai A, Yamamoto M, Fujisawa Y, Kanzaki A, Kuroda S. A variant of the sigma receptor type-1 gene is a protective factor for Alzheimer disease. Am J Geriatr Psychiatry. 2005 13(12):1062-6.
11: Hayashi T, Su TP. Sigma-1 receptors at galactosylceramide-enriched lipid microdomains regulate oligodendrocyte differentiation. Proc Natl Acad Sci U S A. 2004 101(41):14949-54.
12: Inada T, Iijima Y, Uchida N, Maeda T, Iwashita S, Ozaki N, Harano M, Komiyama T, Yamada M, Sekine Y, Iyo M, Sora I, Ujikec H. No association found between the type 1 sigma receptor gene polymorphisms and methamphetamine abuse in the Japanese population: a collaborative study by the Japanese Genetics Initiative for Drug Abuse. Ann N Y Acad Sci. 2004 1025:27-33.
13: Uchida N, Ujike H, Nakata K, Takaki M, Nomura A, Katsu T, Tanaka Y, Imamura T, Sakai A, Kuroda S. No association between the sigma receptor type 1 gene and schizophrenia: results of analysis and meta-analysis of case-control studies. BMC Psychiatry. 2003 3:13.
14: Hayashi T, Su TP. Regulating ankyrin dynamics: Roles of sigma-1 receptors. Proc Natl Acad Sci U S A. 2001 98(2):491-6.
Medical Staff Meeting
Our staff meeting is held on every Tuesday at noon for 1.5 hr. In addition to sharing latest medical information regarding treatments and the operation of the hospital, the meeting also includes followings activities.
Journal club (1 time/month)
Scientific/medical articles are selected and presented by assigned doctors according to their personal interests. Articles recently presented are as follows:
1: Mitochondrial dysfunction as a neurobiological subtype of autism spectrum disorder-evidence from brain imaging-. JAMA Psychiatry. 2014, 71: 665-71.
2: Folate and vitamin B12 status in schizophrenic patients. Journal of Research in Medical Sciences. 2011, Vol16(Suppl1): S437-S41.
3: Rethinking schizophrenia. Nature. 2010. Vol.468. 187-93.
4: Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: systematic review and dose-response meta-analysis of prospective cohort studies. British Medical Journal. 2014, 349:g4490.
5: Community outreach for patients who have difficulties in maintaining contact with mental health services: longitudinal retrospective study of the Japanese outreach model project. BMC Psychiatry. 2014,14:311
6: Effect of bright light and melatonin on cognitive and noncognitive function in elderly residents of group care facilities. JAMA. 2008, 299: 2642-55.
7: Self-help groups reduce mortality risk: A5-year follow-up study of alcoholics in the Tokyo metropolitan area. Psychiatry and Clinical Neurosciences. 2004. 58: 551-7.
Case presentation and discussion (1 time/month)
In- or outpatients treated at Nishikawa hospital are presented and their treatment strategies are discussed. Cases presented recently are as follows:
1: A case of lithium-induced nephrogenic diabetes insipidus actualized following neuroleptic malignant syndrome.
2: Delirium in a very elderly case caused by withdrawal of zolpidem.
3: Case management of a schizophrenic case who is compulsorily hospitalized and his family refuses the payment for medical expenses.
4: A case of anxiety disorder whose physical complaints abolished by paroxetine treatment.
5: Managing antisocial behaviors of a young female inpatient with dissociative disorder.
6: A case of depression who are diagnosed as Asperger syndrome after his hospitalization.
7: Impact of the whole-organization case conference on the management of a severe schizophrenic inpatient.
8: Delirium triggered by a traffic accident.
9: Environmental management for a case of autism spectrum disorder with highly restricted patterns of interest.
10: A case of schizophrenia whose polydipsia is improved by changing antipsychotic drugs.
11: A case of schizophrenia whose sexual function is recovered by switching paliperidone to aripiprazole
Expert opinion (1 time/month)
Senior medical doctors having over 35 years of carrier provide free talks of their experiences, and bring messages to young doctors.
Recent talks:
1: “My personal histories I,” “My personal history II” by Dr. Y.Uchida
2: “My carrier process during 44 years serving as a psychiatrist” by Dr. I. Koga
3: “Hypothesis of etiology of schizophrenia and its animal models” by Dr. T. Nishikawa
4: “Looking back my clinical carrier at Nishikawa hospital I: review of 4 cases of organic brain diseases” by Dr. M. Nishikawa
5: “My personal history” by Dr. S. Matsunaga